Introduction:
A 37-year-old married man with a young child presented with a chief complaint of persistent abdominal discomfort. Concerned about his symptoms, he sought medical attention, leading to a series of investigations that ultimately revealed a diagnosis of metastatic intrahepatic cholangiocarcinoma. This case study follows his journey from diagnosis and ongoing management.
Patient Presentation:
The patient’s journey began with subtle symptoms of abdominal discomfort, prompting him to seek medical evaluation. Despite his relatively young age, our medical team discovered a significant underlying health concern – metastatic intrahepatic cholangiocarcinoma. This diagnosis came as a shock to the patient and his family, as they grappled with the emotional impact and uncertainty surrounding his condition.
Medical History:
Before his cancer diagnosis, the patient had no significant medical history. He was a devoted husband and father, providing financial stability that enabled access to advanced medical care for his condition. This support system would prove invaluable throughout his treatment journey.
Diagnostic Findings:
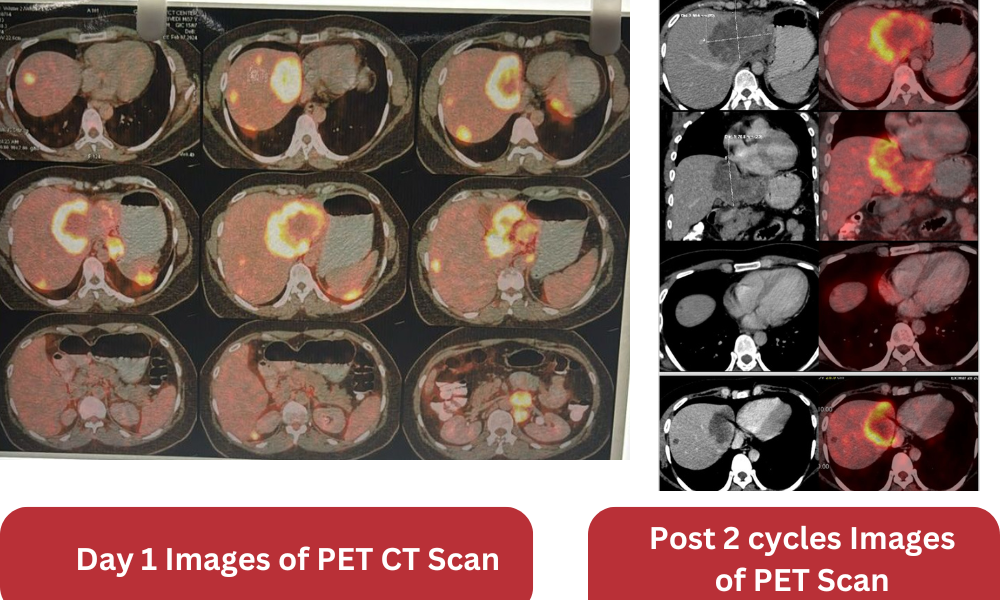
CT scan (6/2/24): Multiple liver lesions noted in both lobes, with the largest measuring 8.5 x 7.5 cm. Lymphadenopathy observed in periportal, peripancreatic, and pan-aortic regions.
PET CT Scan (7/2/24): Hypodense liver lesions at segments II, III, IV, and VI, along with abdominal lymphadenopathy and a subserosal lesion measuring 3 cm.
Liver Biopsy (9/2/24): Confirmed intrahepatic cholangiocarcinoma. Immunohistochemistry positive for CK7 and CK19, negative for CK20, CDX2, and TTF1.
Laboratory Results (6/2/24): Elevated CA 19.9 (111.1 U/ml), AFP-4.58, PSA-0.39, CEA-1.48. Liver function tests within normal limits.
Cardiac Assessment: 2D Echocardiogram (15/2/24): Left ventricular ejection fraction (LVEF) approximately 64%.
Discussion of Management:
Upon diagnosis, our medical team assembled a comprehensive treatment plan tailored to his specific needs. This multidisciplinary approach involved oncologists, surgeons, and other specialists collaborating to devise the most effective strategy. Given the advanced stage of his cancer, the team opted for a combination therapy approach, aiming to maximize treatment efficacy while minimizing adverse effects.
Treatment Approach:
The patient’s treatment regimen comprised a combination of chemotherapy and immunotherapy. This approach combined traditional chemotherapy agents, such as cisplatin and gemcitabine, with cutting-edge immunotherapy drugs like Durvalumab. By targeting cancer cells directly and enhancing the body’s immune response, this treatment strategy aimed to control tumor growth and improve overall survival.
Response to Treatment:
Following the initiation of treatment, our medical team closely monitored his progress through regular imaging studies, laboratory tests, and clinical assessments. While the initial phases of therapy saw fluctuations in tumor markers, subsequent evaluations revealed signs of partial response to treatment. Tumor burden decreased, and markers of disease activity, such as CA 19-9 levels, began to decline, providing hope and encouragement to the patient and his loved ones.
Current Status:
As the patient continues to undergo further cycles of treatment, our medical team remains vigilant in monitoring his progress and adjusting therapy as needed. Ongoing imaging studies and laboratory assessments are essential in evaluating treatment efficacy and disease response. Despite the challenges associated with managing metastatic cancer, there is optimism regarding the patient’s response to therapy and the potential for improved outcomes.
Conclusion:
The collaborative efforts between patients, families, and the healthcare team form the cornerstone of effective cancer management, providing invaluable emotional and psychological support throughout the treatment process.
As the patient continues his journey, maintaining open lines of communication and fostering a supportive environment will be instrumental in addressing the multifaceted needs of both the patient and his loved ones. By prioritizing holistic care and embracing a patient-centered approach, we can navigate the complexities of metastatic intrahepatic cholangiocarcinoma with compassion and resilience, ultimately striving towards improved outcomes and enhanced quality of life.
